What is Discordance?
Guest blog by Nick Birch, FRCS (Orth)
The diagnostic categories of bone density include normal, osteopenia and osteoporosis. The reference level of bone density is that of a healthy 30-year-old adult, an age that is chosen as it represents “peak bone mass” i.e. the best bone density a person can expect to have in normal circumstances. If everyone was the same, it would be expected that they would all have normal bone at the age of 30 and that over time there would be a reduction of bone density with age and in women with the onset of menopause. However, everyone is not the same. There is considerable variation in height, weight, levels of physical activity, diet and background medical conditions. As a result, the three diagnostic categories, which are very much a “one size fits all” set of labels, do not adequately describe the bone health of significant proportions of the population.
Bone density varies with build. People with a higher body mass index have an increased bone density compared to people with a lower body mass index. In women sustaining a low-energy fragility fracture, only a third have a DXA diagnosis of osteoporosis i.e. low bone density. The other two thirds have diagnoses of osteopenia or normal bone density. This demonstrates that it is not just the bone density that determines fractures, but other factors as well. One of the most important of these is bone toughness (bone quality or bone strength). Toughness comes about as a result of repeated impact exercise when the underlying condition of bone is normal i.e. there are no medical reasons for bone to be weak.
For example, a person with a low body mass index who is extremely active will have a low bone density commensurate with their build, but their bone toughness is likely to be good. Therefore, they may be less likely to fracture than an overweight, unfit person who will have better bone density but poor bone quality.
In most people the diagnostic category for the hip and the spine will be the same, but if the T-scores are close to the boundary between diagnostic categories they can be different. This difference is called discordance. But does this mean there is more like to be a fracture in one part compared to the other because one diagnosis is worse than the other? To understand these questions the original definitions of Normal, Osteopenia and Osteoporosis need to be revisited.
Osteoporosis is defined by the World Health Organization (WHO) as: A systemic condition characterized by low bone mineral density (BMD) in the osteoporosis range measured by bone densitometry (T score < -2.5) or a significant fracture risk based on fracture risk assessment e.g. FRAX with or without fragility (low trauma) fractures.
Systemic means affecting the whole body and, in this case, refers to the whole skeleton. Generally, in premenopausal women, it is expected that the bone density of the spine and hips will of the same order of magnitude unless there are specific reasons for them to be different such as playing sport where the impact is taken more on one lower limb than the other.
In postmenopausal women there often is more variation, which can also be the case in people who have specific reasons not to use certain parts of their bodies such as those who have suffered paralysis because of a stroke or an injury resulting in prolonged off-loading of a lower extremity.
When the T-scores fall into the same WHO diagnostic category (normal, osteopenia, osteoporosis) they are defined as being concordant. If they fall into different WHO diagnostic categories, they are discordant.
A minor discordance is defined as T-scores in adjacent WHO diagnostic categories of bone density:
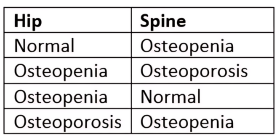
A major discordance is present if either the hip or spine T-score is normal and the other is osteoporotic.
Even if T-scores at hip and in the spine put a woman’s bone density into the same WHO diagnostic category, large differences between T-scores e.g. -2.5 at the hip and -4.7 in the spine need to be explained if there is no clear clinical reason why such a difference exists.
There are several reasons for discordance:
Physiological The skeleton’s adaptive reaction to mechanical strain
Pathophysiological A disease state affecting the skeleton
Anatomical Differences between sites in content of cortical and trabecular bone and/or rate of bone loss
Artefactual The presence of manmade items within the region of interest of the test
Technical Faulty device hardware or software or the technologist’s method of acquiring or analyzing the test
Physiological, pathophysiological and anatomical reasons for discordance refer to clinical variation and they are therefore unrelated to the actual bone density test.
Anatomical reasons include the different distribution of hard (cortical) bone and softer (cancellous) bone in the hip and spine. With advancing age, an increased incidence of degenerative conditions in the spine and hip (e.g. arthritis) can cause errors in DXA analysis leading to discordant results. Other factors include ages of onset of menarche (puberty) and menopause (more discordance with late menarche and early menopause), Body Mass Index (less discordance with obesity) and secondary causes of osteoporosis (chronic inflammatory conditions and long-term use of some medications can predispose to discordance). In addition, some populations that are prone to vitamin D deficiency (women in Muslim communities wearing the Burka and Niqab) show different rates of discordance compared to populations that are more exposed to sunlight.
Artifactual and technical reasons for discordance are the result of equipment calibration and operator error and can be eliminated by strict adherence to correct bone densitometry principles and practice. For DXA the latter include correct patient positioning and interpretation of the x-ray images. Neither of these are relevant for REMS scans.
Six studies published between 2000 and 2014 showed the rates of concordance and discordance as:
Concordance 48% - 58%
Minor discordance 35% - 46%
Major Discordance 2% - 17%
Reference Files:
Summary of studies reporting the rates of T-score concordance and discordance
Details of concordance and discordance rates in studies of DXA performance
In 2023 Young and Birch presented their results of REMS discordance rates showing a minor diagnostic discordance rate of 15%, a numerical discordance rate (i.e. a difference between T-scores of the hip and spine of < 1.0) of 6.5% and a major discordance rate of 0.0%.
If a woman has a DEXA scan showing a major discordance, or a T-score discrepancy of more than 1.0 and she has no obvious reasons for such a result, she should query the DXA result with the local unit. If a reasonable answer is not forthcoming, asking for a second opinion with a bone density scan performed either on a different DXA machine or with alternative technology e.g. REMS, is entirely reasonable and appropriate.