Part 1: Understanding the Impact of Statistics and Databases on Your DXA and REMS Test Results
I’m Active, Eat Right, and Have Never Broken a Bone…Why is my Fragility Score Yellow or Red?!?!?!
Authors:
Kimberly Zambito, MD, Orthopaedic Surgeon and Owner of Qualis Os
Dr Nick Birch FRCS (Orth), Consultant Spine and Bone Health Specialist
Andrew Bush, MD, Orthopaedic Surgeon
Why is it that some people who do everything right still have a dismal T- score or Fragility Score? The answer to this question has many facets, but the underlying science is based on statistics, population health and screening for diseases.
DXA is considered the “gold standard” for screening for osteoporosis. Since DXA is considered the current gold standard, all other technologies used to evaluate bone mineral density (BMD) are compared to DXA. REMS is an ultrasound technology used in the evaluation of BMD that has been extensively verified against DXA. However, it is unique in being able to measure bone quality of the hips and spine through the fragility score (FS).
BMD is expressed either as g/cm2 or g/cm3. The first represents the value of an area of a bone surface that is being examined and the second the volume of the relevant bone. Areal values are obtained from DXA and REMS machines and volumetric values are obtained through a CT scan. In general, DXA and REMS are the more commonly used technologies, so your results are more likely to be reported as g/cm2.
The REMS Fragility Score is a measure of the structural quality of bone that is independent of the BMD. It measures bone toughness, which has been established as the most important contributor to future fracture risk. Bone quality, or toughness, is comprised of bone density, microarchitecture, shape, along with other variables.
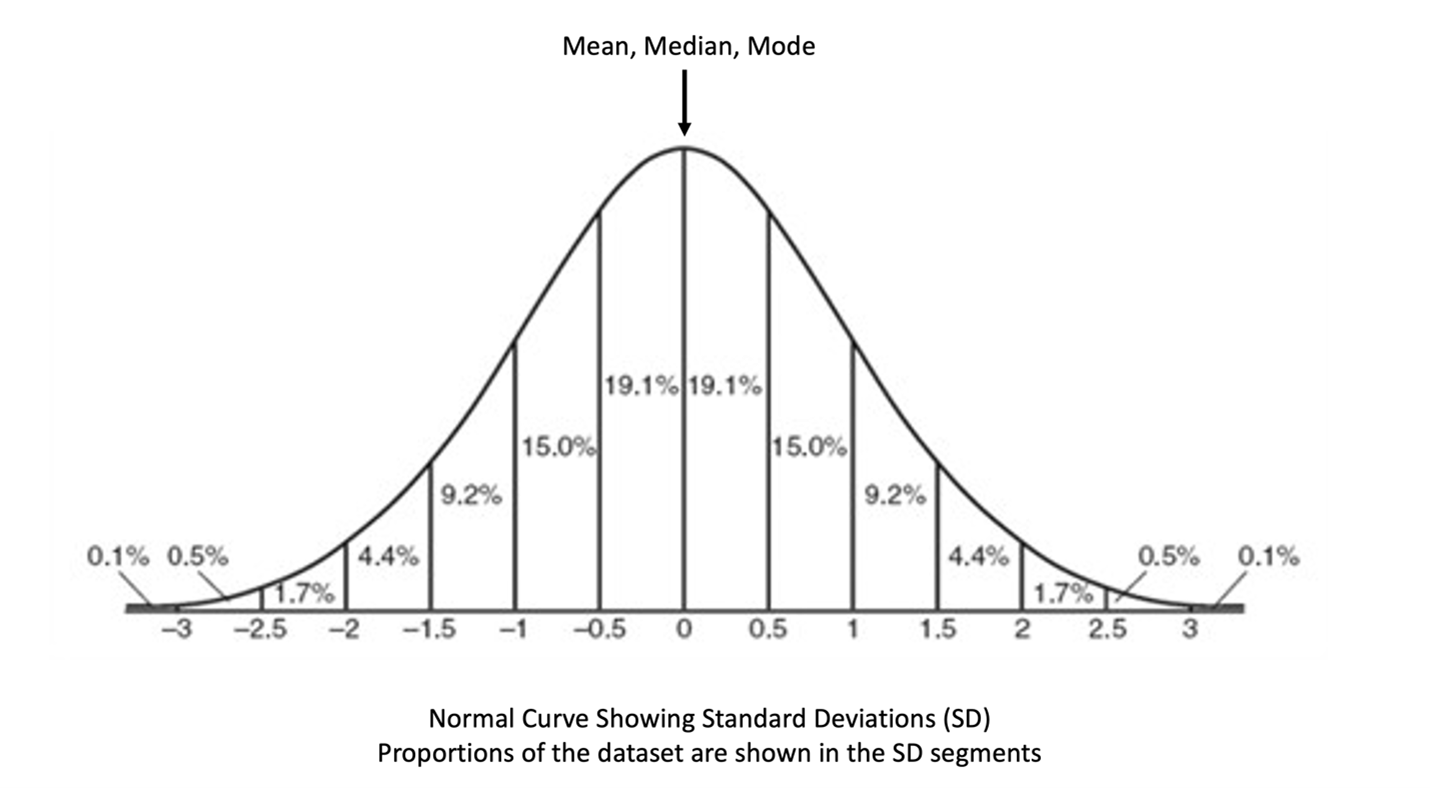
Whenever a screening technology is developed, data from a large number of people who have had the test are accumulated and stored in a database. As that database is progressively built, it comes to represent the variety of values of the test the target population will have. The larger the database, the more representative it will be of the general population. When we look at a “picture,” or graph, representing these data, most often it is in the form of a bell-shaped curve. This is called a “normal distribution” / “normal curve”. Most of the data points fall within a central band and clusters of values taper symmetrically on either side, creating the bell-shape.
If we examine various parts of the curve the middle value is called the “median”. The “mean” is the average of all the datapoints and the “mode” is the most frequent value. In a perfect bell-shaped curve, all three fall at the highest point of the curve.
Normal distribution curves can be subdivided into equal segments which are called “standard deviations.” These represent the "spread" of the data where a larger standard deviation indicates a wider bell-shaped curve, and a smaller standard deviation indicates a narrower curve.
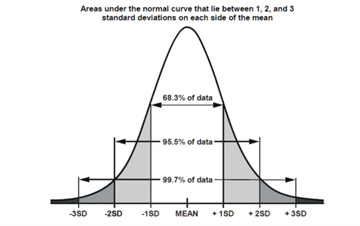
In general, when we interpret the information in a bell-shaped curve, we follow the “68-95-99” rule. Approximately 68% of data falls within one standard deviation of the mean, 95% within two standard deviations, and 99.7% within three standard deviations.
How is this applied to information in your DXA or REMS scan results for BMD? The first value to look at is your “Z score”. This represents the difference between your bone density and the average bone density for people of your age who are the same gender and ethnicity as you. If your BMD (in g/cm2) is close to the middle (or mean), then your Z-score will be close to “0”. If your BMD in g/cm2 falls away from the middle, it will be given a Z-score that shows how far away from the average your BMD is. Z-scores can be positive or negative depending on whether your bone density is above or below average for your age. Therefore, if your Z-score is -1.0, your BMD is 1 standard deviation lower than the average population for your age, gender, and ethnicity. If your Z-score is -1.5, then your BMD is 1.5 standard deviations lower than the average population for your age, gender, and ethnicity. The same applies with positive Z-scores with +1.0 being 1 standard deviation above average and +1.5 being 1.5 standard deviations greater than the average population for your age, gender, and ethnicity.
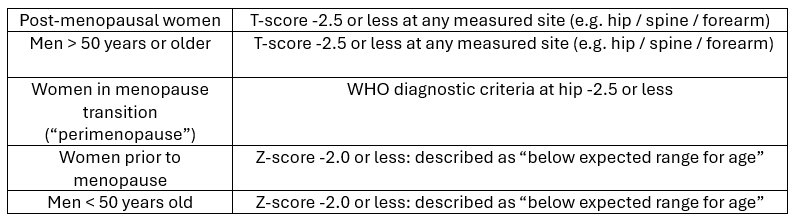
At this point you might wonder why there is all this talk about Z-scores when everyone knows that bone density is expressed as T-scores. The reason is because the two types of score show bone density by reference to different populations. As we have said, Z-scores compare you to people your age who are the same gender and ethnicity. T-scores compare your BMD to the BMD of young healthy adults, who happen to be white women between the ages of 20 and 29 years, irrespective of your gender and ethnicity. The intent of using T-scores is to express how much bone loss has occurred since the age of 30 in the general population and from these values the World Health Organisation (WHO) diagnostic categories of “normal”, “osteopenia” and “osteoporosis” are derived. The table below shows how a diagnosis of osteoporosis is made in different groups of people.
Considering post-menopausal women, their T-scores show how much difference there is between their bone density and the bone density of young healthy white women, up to the age of 30, which is used as a reference. By 30 years of age, most women have reached “peak bone mass” which means they have the best bone density of their lives. From 30 to 40 years, bone mass is expected to remain stable, but after 40 there is a progressive loss of bone mass which is most rapid at the time of menopause and for the first 10 years afterwards. Unfortunately, most women do not know what their BMD or T-scores were at the age of 30 and if you do not know your starting point or baseline, how can it be assumed that you have lost a large amount of bone density by the time of the menopause? What if your baseline was low? Is it possible you have not lost much bone since you were 30? Is it possible you have lost bone density no more than anyone else through the aging process? After the age of 40 average bone loss is 0.5-1.0% per year except for women during the first decade after menopause when it can be as high as 2% per year (more statistical information from a database). How can we then understand who might be at risk of future fractures because of a deterioration of bone health after the age of 30? The simple answer is: Screening.
Screening is a process that involves checking for a disease or condition in people who appear healthy. So, screening for osteoporosis means we need to measure the bone density of people in the community by appropriate tests from which their T- and Z-scores are derived. Some people will have osteoporosis, and the test will show that to be the case because their T-scores or Z-scores are below the thresholds that define the diagnosis. These are “True Positive” results. Others won’t have osteoporosis, and the test will also show that to be the case as the T- or Z-scores will be above the diagnostic threshold (“True Negative” results). However, the test might not be completely accurate which means it could show a person who has osteoporosis as not having the condition (“False negative” result) or vice versa, a person who doesn’t have osteoporosis is shown as having the condition (“False Positive”) result. The accuracy of any screening test depends on the relationship between the four possible outcomes. The higher the proportion of true positive and true negative cases the more accurate the test. Why is this important?
When we identify people at higher risk of having a disease, then we can offer preventive measures or treatment. Let’s look at an example of a screening tool used in general medicine. An electrocardiogram (EKG) is used to evaluate electrical impulses of the heart and can be useful in identifying irregular heart rhythms which can be life threatening. Bradycardia is defined as a low heart rate. Let’s say a cardiologist is reviewing an EKG. The EKG demonstrates a very low heart rate of 44 beats per minute. Is this a cause for concern? The answer is “it depends.” If this person is a 30-year-old endurance athlete, then there is, most likely, no cause for concern. If this person is an 80-year-old on cardiac medication who is feeling dizzy, then yes there is cause for concern. The information from these screening tools must be interpreted within the appropriate context.
DXA and REMS are technologies we use to screen for osteoporosis, and by implication, fracture risk. However, knowing a person’s T-score or Z-score in isolation is only part of the picture and the information gained from these tools does not define a person. The results from DXA and REMS are in essence “medical statistics” that need to be properly interpreted by a trained professional who knows how to apply the information in the correct context of your general health, specifically as it applies to your bone health. Remember, you are more than your DXA and REMS results. There is an ENTIRE you!
Coming soon - Part 2: Understanding the Impact of Databases on Your Fragility Score and Fracture Risk